History:
A 55-year-old woman presented to the ED with a 1-week complaint of left knee pain, swelling, erythema, and warmth to touch. She also reported tactile fevers and chills without any other constitutional symptoms. She did note a recent history of a left total knee replacement the year prior, as well as a prosthetic infection of the same joint with operative wash out two months prior to the current visit.
Examination:
On physical exam there was a midline scar along the anterior aspect of the left knee consistent with a recent surgery. The patella was midline and there was no obvious bony deformity. There was some generalized erythema of the knee, along with fluctuance of the suprapatellar region. The knee was tender to palpation along the medial joint line and unable to be fully extended.
Emergency Department Course:
The ED physicians were concerned for septic arthritis and an emergent consult to Orthopedic Surgery was made. The orthopedic surgeon attempted to perform three blind joint aspirations without success. The consulting physician advised discharge to home given his low suspicion for a septic joint due to the lack of joint aspirate. The ED physician remained concerned and requested an ultrasound evaluation of the knee.
Radiographs:
None
Ultrasound Examination of the Knee
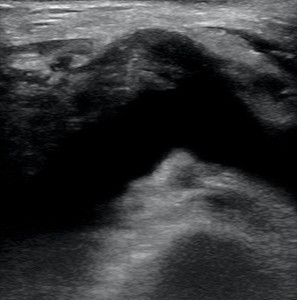
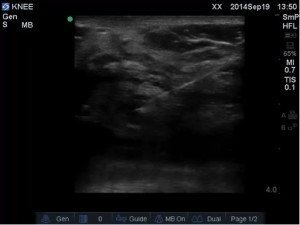
A high frequency linear transducer was used with a musculoskeletal setting. The probe was placed in a transverse plane over the anterior knee just proximal to the patella. The following image was obtained:
Ultrasound examination of the knee clearly showed a joint effusion of the left knee. The effusion is noticeable as an anechoic distention of the suprapatellar recess.
Procedure:
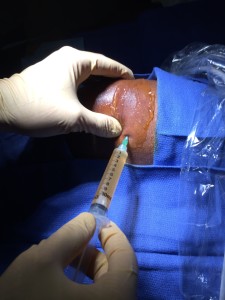
The patient was placed in the supine position with the knee in slight flexion. The knee was prepped and draped in sterile fashion and local anesthetic was initially injected in preparation for the procedure.

A 10cc syringe with 18-gauge angiocatheter was then used to enter the joint space under ultrasound guidance.
Joint aspirate was obtained and sent for fluid analysis.
Conclusion:
Synovial fluid analysis confirmed the presence of a septic effusion with fluid culture positive for Streptococcus Agalactiae. The patient was taken to the OR that day for a Stage 1 revision of her left TKR, at which time all implants were taken out and a temporary antibiotic spacer was placed. The patient was discharged to a sub-acute rehab facility with a PICC Line and antibiotics. She continues to remain in stable condition with no further complications at this time.
Take Home Points:
- Consider using a long angiocatheter when performing a joint aspiration or injection. The catheter can be left in place and the needle removed. This not only minimizes the likelihood of the needle exiting the joint space, but also simplifies repeated aspirations or even an aspiration followed by joint injection of anesthetic/steroid for therapeutic taps.
- When performing your initial ultrasound evaluation for a joint effusion, remember that too much pressure can collapse the joint recess and result in difficulty visualizing the fluid.
- If the joint is placed in a position of flexion, small joint effusions may only be present superolateral to the patella. If the joint is fully extended, a small joint effusion will likely only be present along either the medial or lateral border of the patella.
- Ultrasound vs. Blind Approach: So what does the data show? In a study published in 2009 in the Journal of Rheumatology, Sibbit et Al. found that ultrasound not only increased the detection of a joint effusion by nearly 200% but also the volume of fluid aspirated. Furthermore, ultrasound guidance may also affect the clinical outcome, including decreased levels of pain experienced during the procedure. Does sonographic needle guidance affect the clinical outcome of intraarticular injections?