History:
20 year old male presents with a one hour history of left testicular pain and swelling which began acutely after he got out of the shower. He denies dysuria, urethral discharge or trauma. He states that this has never happened before and says this is the worst pain he has ever had in his entire life. Since arriving to the ED he has become nauseous and has vomited several times.
Exam:
Afebrile, vitals signs stable.
GU exam reveals a horizontal lie to his left testicle with significant tenderness. Absent cremasteric reflex. Remainder of the GU exam is normal. No inguinal lymphadenopathy and the abdominal exam is unremarkable.
Evaluation and Management:
The patient was seen nearly immediately after arrival via EMS and we were concerned for a possible testicular torsion and therefore elected to perform a manual detorsion procedure. While preparing for this we grabbed the ultrasound machine, paged urology and had the nurse place a peripheral IV to administer 1mg of Dilaudid. Although emergency point of care (POC) scrotal ultrasound (US) is not a standard US exam done in the Emergency Department (ED), we decided to attempt the exam to see if there was blood flow to the affected testicle prior to attempted detorsion and then to repeat the exam after the procedure.
US image Review:
POC Scrotal US was performed using the high frequency linear probe. The bilateral testes were scanned in transverse and sagittal planes:
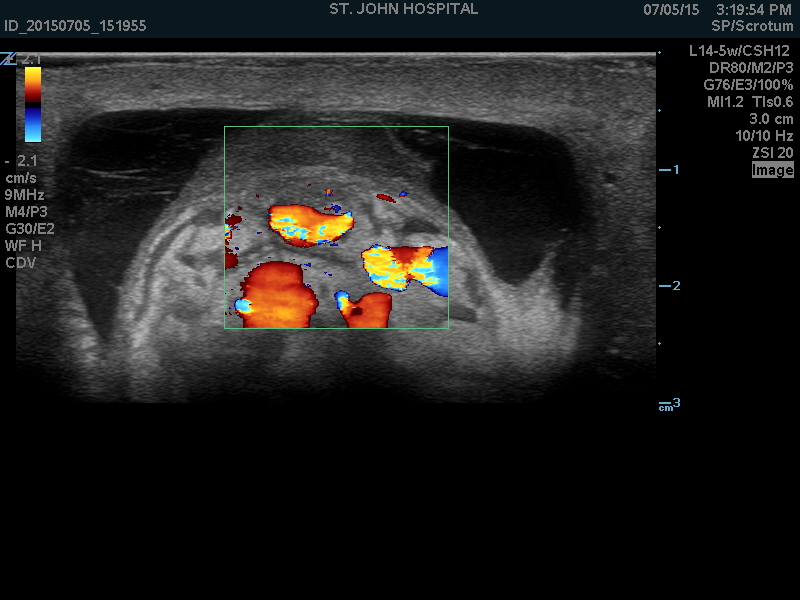
The right hemiscrotum was imaged first to help optimize the settings, and was found to be normal (Figure 1 Normal Right Testicle). The left side was remarkable for a small amount of fluid surrounding the testicle (hydrocele). Color flow doppler imaging was obtained to assess for the presence of blood flow to the testis. The left side imaging showed no flow to the left testicle (Figure 2 Left Testicle).
Given the history, exam and POC US findings, we now felt certain the patient had testicular torsion (TT) and proceeded with manual detorsion. The left testes was rotated 180 degrees in a medial to lateral direction. Upon completion of this rotation the patient expressed complete relief of pain. We then repeated the scrotal US to assess if there was now blood flow to the testicle (Figure 3 Left Testicle s/p detorsion). Once color flow was noted to be present on the left, we then used pulse wave (PW) Doppler to document arterial and venous flow to the left testes.
Urology arrived shortly after scheduled the patient for operative repair and requested a radiology performed US. This exam as interpreted as normal other than a small hydrocele. The patient was taken to the OR for an orchiopexy within 90 minutes of his arrival in the ED.
Summary and Take Home Points:
- There have not been any prospective studies on POC scrotal US performed by emergency physicians; but a very similar case was published as a case report in Academic Emergency Medicine in 2009. Here US was also used to aid in manual detorsion. In this case, the detorsion required 540 degrees of rotation. The US was a particularly important adjunct because several rotations were required and US allowed for intermittent assessment of flow in between rotations (1).
- Testicular torsion is a time sensitive diagnosis. The chance of salvage declines rapidly after 6 hours from greater than 90% to less than 25% after 12 hours (2). “Time is Testicle (i.e. fertility)”.
- Most history and exam features that are used in the evaluation of acute testicular pain have been disproven to some extent. Many feel that absence of the cremasteric reflex is the most sensitive finding for torsion, but in fact some studies have shown preservation of the cremaster reflex in 29- 40% of patients with confirmed TT (3). Utilizing POC scrotal US to diagnose TT by demonstrating a lack of blood flow can save the patient much needed time spent waiting for radiology to perform a scrotal US prior to consultation with urology in atypical cases.
- As demonstrated in our case as well as the attached case report, POC scrotal US can aid in manual detorsion especially in cases where a significant amount of rotation is required. A manual detorsion procedure can restore blood flow and improve testicular salvage.
- We are not suggesting that an emergency physician performed POC scrotal US be used to “rule out” torsion. We are suggesting that POC US be used to support your suspicion based on history and physical exam. Doing so might help you save a testicle!
References:
- Bomann JS & Moore C. Bedside Ultrasound of a painful Testicle- Before and After Manual Detorsion by an Emergency Physician. Acad EM 2009
- Wang and Scoutt. Testicular Torsion and Manual Detorsion. Ultrasound Quaterly. Vol 29, no 3. 2013
- Mellick, Torsion of the Testicle. It’s time to Stop rolling the Dice. Pediatric Emergency Care. Vol 28, no 1. 2012.